Last week, researchers at the West Virginia University Rockefeller Neuroscience Institute reported that by using focused ultrasound to open the blood-brain barrier, they
improved delivery of a new Alzheimer’s treatment and sped up clearance of the sticky plaques that are thought to contribute to some of the cognitive and memory problems in people with Alzheimer’s by 32%.
For this issue of The Checkup, we’ll explore some of the ways scientists are trying to disrupt the blood-brain barrier.
WVU ROCKEFELLER NEUROSCIENCE INSTITUTE
In the West Virginia study, three people with mild Alzheimer’s received monthly doses of aducanumab, a lab-made antibody that is delivered via IV. This drug, first approved in 2021, helps clear away beta-amyloid, a protein fragment that clumps up in the brains of people with Alzheimer’s disease. (The drug’s approval was controversial, and it’s still not clear whether it actually slows progression of the disease.) After the infusion, the researchers treated specific regions of the patients’ brains with focused ultrasound, but just on one side. That allowed them to use the other half of the brain as a control. PET scans revealed a greater reduction in amyloid plaques in the ultrasound-treated regions than in those same regions on the untreated side of the brain, suggesting that more of the antibody was getting into the brain on the treated side.
Aducanumab does clear plaques without ultrasound, but it takes a long time, perhaps in part because the antibody has trouble entering the brain. “Instead of using the therapy intravenously for 18 to 24 months to see the plaque reduction, we want to see if we can achieve that reduction in a few months,” says Ali Rezai, a neurosurgeon at West Virginia University Rockefeller Neuroscience Institute and an author of the new study. Cutting the amount of time needed to clear these plaques might help slow the memory loss and cognitive problems that define the disease.
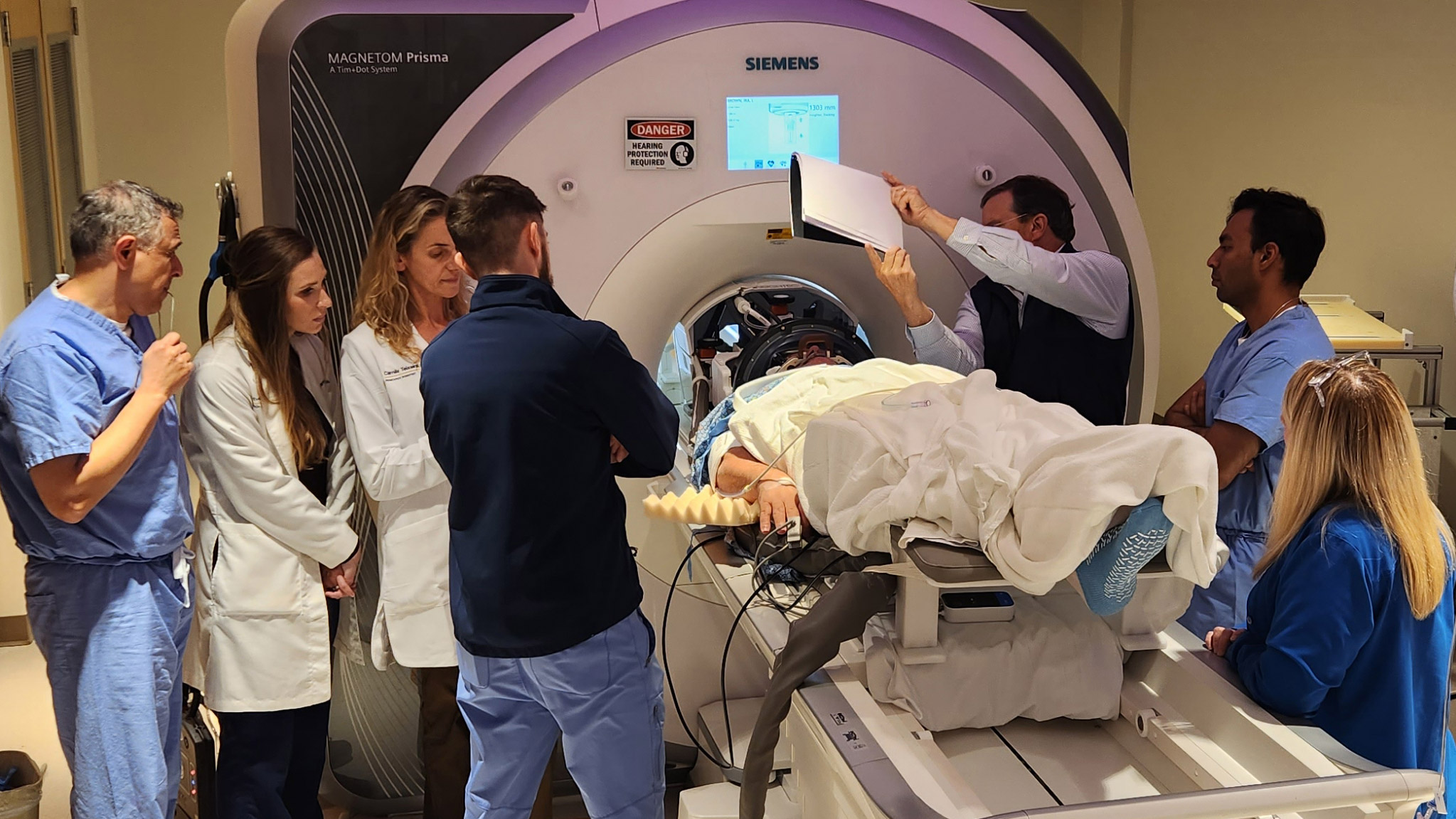
The device used to target and deliver the ultrasound waves, developed by a company called Insightec, consists of an MRI machine and a helmet studded with ultrasound transducers. It’s FDA approved, but for an entirely different purpose: to help stop tremors in people with Parkinson’s by creating lesions in the brain. To open the blood-brain barrier, “we inject individuals intravenously with microbubbles,” Rezai says. These tiny gas bubbles, commonly used as a contrast agent, travel through the bloodstream. Using the MRI, the researchers can aim the ultrasound waves at very specific parts of the brain “with millimeter precision,” Rezai says. When the waves hit the microbubbles, the bubbles begin to expand and contract, physically pushing apart the tightly packed cells that line the brain’s capillaries. “This temporary opening can last up to 48 hours, which means that during those 48 hours, you can have increased penetration into the brain of therapeutics,” he says.
Focused ultrasound has been explored as a method for opening the blood-brain barrier for years. (We wrote about this technology way back in 2006.) But this is the first time it has been combined with an Alzheimer’s therapy and tested in humans.
