The software being tested comes from Vara, a startup based in Germany that also led the study. The company’s AI is already used in over a fourth of Germany’s breast cancer screening centers and was introduced earlier this year to a hospital in Mexico and another in Greece.
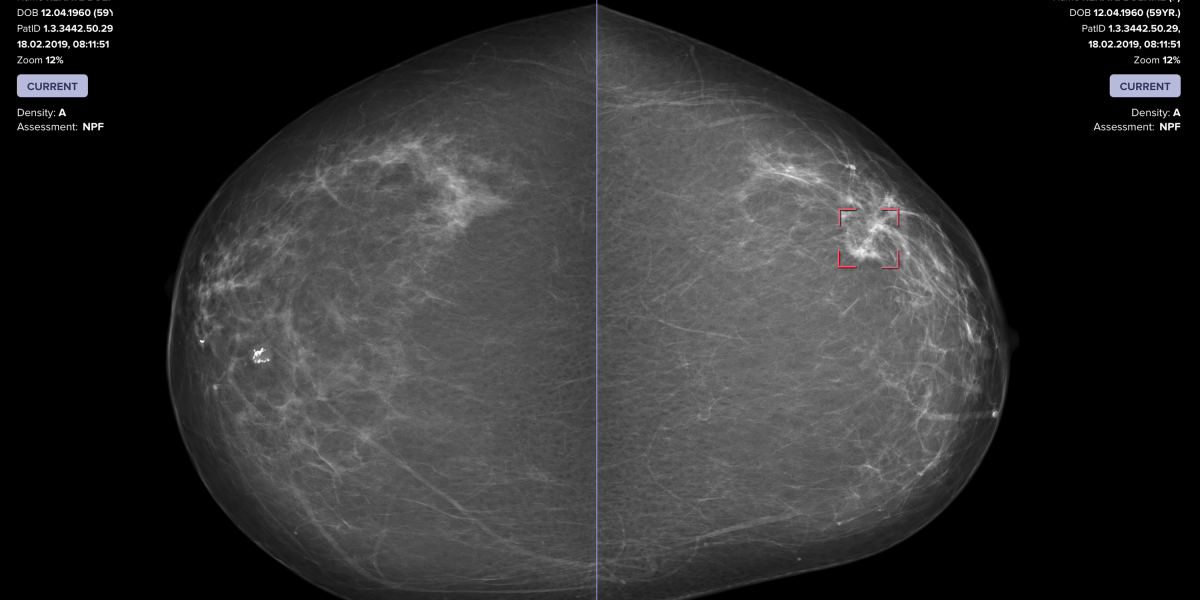
The Vara team, with help from radiologists at the Essen University Hospital in Germany and the Memorial Sloan Kettering Cancer Center in New York, tested two approaches. In the first, the AI works alone to analyze mammograms. In the other, the AI automatically distinguishes between scans it thinks look normal and those that raise a concern. It refers the latter to a radiologist, who would review them before seeing the AI’s assessment. Then the AI would issue a warning if it detected cancer when the doctor did not.
“In the proposed AI-driven process nearly three-quarters of the screening studies didn’t need to be reviewed by a radiologist, while improving accuracy overall.”
Charles Langlotz
To train the neural network, Vara fed the AI data from over 367,000 mammograms—including radiologists’ notes, original assessments, and information on whether the patient ultimately had cancer—to learn how to place these scans into one of three buckets: “confident normal,” “not confident” (in which no prediction is given), and “confident cancer.” The conclusions from both approaches were then compared with the decisions real radiologists originally made on 82,851 mammograms sourced from screening centers that didn’t contribute scans used to train the AI.
The second approach—doctor and AI working together—was 3.6% better at detecting breast cancer than a doctor working alone, and raised fewer false alarms. It accomplished this while automatically setting aside scans it classified as confidently normal, which amounted to 63% of all mammograms. This intense streamlining could slash radiologists’ workloads.
After breast cancer screenings, patients with a normal scan are sent on their way, while an abnormal or unclear scan triggers follow-up testing. But radiologists examining mammograms miss 1 in 8 cancers. Fatigue, overwork, and even the time of day all affect how well radiologists can identify tumors as they view thousands of scans. Signs that are visually subtle are also generally less likely to set off alarms, and dense breast tissue—found mostly in younger patients—makes signs of cancer harder to see.
Radiologists using the AI in the real world are required by German law to look at every mammogram, at least glancing at those the AI calls fine. The AI still lends them a hand by pre-filling reports on scans labeled normal, though the radiologist can always reject the AI’s call.
Thilo Töllner, a radiologist who heads a German breast cancer screening center, has used the program for two years. He’s sometimes disagreed when the AI classified scans as confident normal and manually filled out reports to reflect a different conclusion, but he says “normals are almost always normal.” Mostly, “you just have to press enter.”
Mammograms the AI has labeled as ambiguous or “confident cancer” are referred to a radiologist—but only after the doctor has offered an initial, independent assessment.
